I promised I'd get here sooner or later - my little blog of unabashed complaint.
I promised I'd get here sooner or later - my little blog of unabashed complaint.I am fed up with the medical profession. Not only fed up, but disillusioned and feeling as if it is impossible to be an effective advocate for myself, and more frighteningly, for my children.
Gee, I like the sound of that: CHILDREN. Plural.
I digress.
What I was getting at was Silas' birthstory including all the highs, the lows and the final unsettling understanding.
Whilst in the hospital this last time, I had the misfortune of witnessing first-hand the problems associated with miscommunication starting from the moment we showed up for preadmission testing.
Not only was I sent to the wrong place, but no one seemed to realize I was even pregnant. Laughable, maybe ... but a sign of things to come?
When we checked in at the hospital for the appointed B-day, the doctor was running an hour late. Not a big deal, as doctors have emergencies, their appointments routinely get backed up. Of course it doesn't seem right that my surgery was scheduled for 5 p.m. on the hottest day of the summer and I'm not allowed to take anything by mouth (not even ice chips) for 10 hours prior. I said it jokingly to the admitting nurse: scheduling this after regular office hours is just "mean." She probably knew I wasn't really joking.
Of course when the doctor arrives, all possible transgressions are forgiven. She is smiling and reassuring. She tells me what I can expect. The baby is going to be a tad early, so there's the possibility -- in addition to the Down scare and the hydronephrosis -- that he may have to spend some time in the Neonatal Intensive Care Unit. If that happens, she counsels, it's for the best, really. He'll get the best care there.
She knows my biggest concern is about the Down potential, and tells me that she's called in a NICU specialist to examine the baby right after delivery, but that it's possible that we won't be able to tell conclusively until chromosomal tests are examined. It doesn't matter, I am relaxed now. I am resigned to accepting anything.
I walk to the operating room.
Things are different this time than they were with Annabel. The anesthesiologist will perform a spinal (not an epidural). I shiver from the cold even though a nurse has layered me in warmed blankets. After the spinal is in place, I'm helped down on the table, arms out but no warming pillows this time. A blind is drawn up so we can't see the surgeons. The anesthesiologist gives me drugs for nausea and puts an oxygen mask on my face. He pinches me on the upper torso and asks me if I feel it. I tell him I do. He pinches me just below my shoulder and asks if the two pinches feel identical. They do not.
We proceed.
There is talking, but I can't hear. This time I'm not interested. I've decided to trust they will tell me anything I need to know.
Jed is holding my right hand, the anesthesiologist is working around my left.
I feel pressure and wonder if they've started cutting. I imagine the process. It takes longer than I remembered and yet it is over in minutes. I feel chest pressure and look away from Jed and toward the doctor. He asks me if I'm alright.
I say yes. The pressure seems to knock a recollection free. More pressure. More rocking.
I remember how hard it seems to wriggle the babies free from their comfortable lodgings.
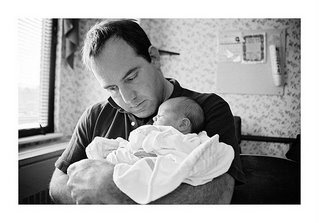
And then the doctor asks Jed if he wants to stand up. He does, and the first thing he reports is all the hair. The kid has a good head of hair.
Then the best sound ever ... crying. Screaming really. Angry put-me-back wails from a little, purple boy.
I crane my neck around to see the nurses working on him.
The high-risk pediatrician breezed past me and asked my age. When I told him, he said the concern is Down syndrome? Jed answered in the affirmative.
"Well he's peeing alright," Jed laughs as our son urinated on the doctor and his pricey stethoscope the moment he stepped up to the bassinette. And a few moments later the doctor, Q-tip in hand and trying to dry out his listening device, tells me he's absolutely positive the kid does not have Down syndrome.
The good news. He's healthy.
The bad news .... hmmmmm. You seem to be bleeding a lot more than 'normal.'
And with that my recovery began. For the next two hours a very attractive PACU nurse named Jennifer checked my vital signs, blood oxygen levels and pressed on my abdomen looking for signs of ... well I don't know really. Excessive bleeding? Temperature that wouldn't elevate? Vomiting?
She told me that while the surgeon and later ordered the placenta to be sent for testing "just because she could," the team had already discarded it when she said earlier it looked fine.
I suppose I should have thought about the Mercury in Retograde thing again, but I didn't. I let it go. I'd convinced myself not to worry.
I had it all. Jennifer, worried, even called the assisting doctor back to check the incision, which she thought was bleeding too much. He applied a compression bandage and called it a night. She sat with me, raised my head and lowered it, helped me latch the baby on to nurse for the first time and told me that she herself had had a miscarriage this year. Jed and I liked her immensely.
I was worried about a transfusion, which she said was a rare occurance before I even mentioned the possibility.
By the time I got to my assigned room in maternity, I was feeling tired but better.
Silas surprised me by being a three-hour sort of boy. Every three hours the nursery staff wheeled his little cart to my room and told me I had a "hongry" boy. Inside the plexigas bassinette was a wide-eyed baby silently opening and closing his mouth like a fish.
The next morning the IV and the cather came out, but I was surprisingly tired. I hoped it was the drugs, and as the day wore on I started to feel better. I had thought that a planned section -- without labor -- would have been a cake walk.
The first face I saw was the mid-wife who told me of the hydronephrosis. I felt guilty for writing about her, namelessly of course, in the newspaper. She was still smiling, though. She checked my incision, saw the compression bandage and asked me when the surgery took place. She asked if it was 7 a.m. or p.m.
P.M. I told her.
She decided she was going to leave the bandage in place for a while longer.
Then, I swear, not 10 minutes later a resident came in a took it off. No questions. Didn't care to inquire about surgical times or the reason it was placed on there to begin with. He then examined the staples and observed some of them "weren't really holding anything together."
So he removed two and replaced them with steri strips.
I asked if he was going to replace the bandage. He hemmed and hawed.
Finally he agreed to put a bandage on the wound.
After he left the midwife came flying back into the room, having heard him in the hallway telling a nurse to get another dressing for me. She was as perplexed as I was, and It was evident that mister doctor man didn't much care for anything a midwife had to offer.
All I could think was How are you supposed to advocate for yourself when you have neither a medical education nor any understanding of procedure. Since "everyone has their own way of doing things: " ... some doctors use michele clips, some use staples. ... Some take the staples out on the day you are released some leave them in until you go for an incision check at your doctors' office a week or two later," a nurse mid-wife later told me.
Nurse after nurse, mid-wife after mid-wife -- but sadly NONE OF MY DOCTORS -- told me one after another that the incision was "not the best they'd ever seen."
And still no answers for me. How do I take care of this? I can't even stand to look at it. Will it get infected? Do I need antibiotics? When will it heal?
I ended up going to see my doctor two days after my release from the hospital to find out before I went mad with fear.
She prescribed antibiotics as a precaution, showed me how to clean and dress it and assured me it would heal nicely and faster than I would imagine.
I left feeling a little better, but ultimately still wondering how is it possible to get to this place before I get to the dark place?
How do you get straight answers from the myriad of people you meet in a hospital.
They're all asking you the same questions, while they tell you different things.
One of the best experiences I've had with a medical professional was the time one asked me to tell him what I understood. When I told him, he could tell me where I misunderstood, too.
I know that I should be happy. That all birthstories include moments of terror and pain and confusion. Because no one is perfect and doctors are not deities. I left the hospital with a wonderful, healthy infant and for that I am eternally grateful.
But I also think my experience, and ultimately every patient's experience, could be better. And I think it should be better.
What bothers me, too, is that I may have to make decisions that go against the recommendations of doctors. That's not a popular tack to take when dealing with people who think they know best. Who think going against their know-how is reckless or akin to child endangerment.
Already I've made my first decision for Silas based on my cumulative hospital experiences. No circumscision.
Jed wasn't so convinced that we should risk the potential for "something to go wrong later on," and was leaning toward the proceedure. I had waffled and told him it was to be his decision to make. But then I took it back.
After being there for three days, and wanting to get answers or even a doctor to look at me, and feeling completely at the mercy of people whom I suspect would rather be golfing, I was convinced of one thing: No more unnecessary surgeries. Not now, not ever.